Scaling Enterprise AI with Anthropic Agent Skills: Architecture and Best Practices
For the past two years, AI development has followed a deceptively simple playbook: stuff everything into the prompt. The logic seemed sound, if Claude can
Techkraft helps healthcare payers optimize data integration and processing, enabling more efficient claims management, improved risk adjustment, and streamlined operations. Our solutions ensure that healthcare payers can handle large volumes of data, comply with regulatory changes, and deliver accurate, timely insights that improve member outcomes. We build data pipelines that support your data strategy and drive operational efficiencies, while ensuring compliance with evolving federal programs.
Challenge 1Data Complexity
Healthcare payers manage vast, diverse data from claims, patient records, pharmacies, and third-party sources. Integrating these into a unified, reliable system is a major challenge.
Solution 1Custom Data Pipelines
We design and optimize data pipelines that integrate claims, patient, and external data, enabling efficient management and actionable insights for claims, risk adjustment, and reporting.
Challenge 2Regulatory Compliance
Adapting to constantly evolving healthcare regulations — from CMS rules to ICD-10 updates and value-based care requirements — demands continuous oversight and system updates.

Solution 2Compliant Operations
Our solutions ensure all data processing and reporting align with current CMS guidelines and other healthcare regulations.
Challenge 3Risk Adjustment Efficiency
Accurate, timely risk adjustment is essential for fair reimbursements and population health management. Without a robust data infrastructure, processing claims and risk scores efficiently becomes difficult, increasing delays and errors.
Solution 3Scalable Data Solutions
Built to scale, our platforms handle billions of records daily, streamlining claims processing, risk adjustment, and operational workflows to help payers manage costs effectively.
Challenge 1Data Complexity
Healthcare payers manage vast, diverse data from claims, patient records, pharmacies, and third-party sources. Integrating these into a unified, reliable system is a major challenge.
Solution 1Custom Data Pipelines
We design and optimize data pipelines that integrate claims, patient, and external data, enabling efficient management and actionable insights for claims, risk adjustment, and reporting.
Challenge 2Regulatory Compliance
Adapting to constantly evolving healthcare regulations — from CMS rules to ICD-10 updates and value-based care requirements — demands continuous oversight and system updates.
Solution 2Compliant Operations
Our solutions ensure all data processing and reporting align with current CMS guidelines and other healthcare regulations.
Challenge 3Risk Adjustment Efficiency
Accurate, timely risk adjustment is essential for fair reimbursements and population health management. Without a robust data infrastructure, processing claims and risk scores efficiently becomes difficult, increasing delays and errors.
Solution 3Scalable Data Solutions
Built to scale, our platforms handle billions of records daily, streamlining claims processing, risk adjustment, and operational workflows to help payers manage costs effectively.
Measure and analyze provider performance based on cost efficiency, clinical outcomes, patient satisfaction, and adherence to care protocols. These insights help healthcare payers identify high-performing providers, address gaps in care delivery, and support value-based contracting initiatives.
Monitor health indicators, social determinants of health, and clinical disparities across member populations. This enables targeted intervention strategies, proactive care management, and improved health outcomes for high-risk or underserved groups.
Evaluate healthcare utilization patterns, costs, service trends, and care effectiveness by analyzing claims data. This helps payers identify cost drivers, detect fraud, forecast future demands, and optimize network management and resource allocation.
Assess member risk profiles by analyzing demographic, clinical, and claims data to support accurate risk scoring and ensure fair, data-driven financial arrangements. This enhances reimbursement accuracy and helps organizations comply with regulatory requirements.
Deliver interactive, real-time dashboards and reports that empower stakeholders to access actionable insights. Our reporting tools support filtered views, drill-down capabilities, and dynamic data visualizations, enabling data-driven collaboration and faster decision-making.

Measure and analyze provider performance based on cost efficiency, clinical outcomes, patient satisfaction, and adherence to care protocols. These insights help healthcare payers identify high-performing providers, address gaps in care delivery, and support value-based contracting initiatives.
Monitor health indicators, social determinants of health, and clinical disparities across member populations. This enables targeted intervention strategies, proactive care management, and improved health outcomes for high-risk or underserved groups.
Evaluate healthcare utilization patterns, costs, service trends, and care effectiveness by analyzing claims data. This helps payers identify cost drivers, detect fraud, forecast future demands, and optimize network management and resource allocation.
Assess member risk profiles by analyzing demographic, clinical, and claims data to support accurate risk scoring and ensure fair, data-driven financial arrangements. This enhances reimbursement accuracy and helps organizations comply with regulatory requirements.
Deliver interactive, real-time dashboards and reports that empower stakeholders to access actionable insights. Our reporting tools support filtered views, drill-down capabilities, and dynamic data visualizations, enabling data-driven collaboration and faster decision-making.


Build and manage scalable pipelines for seamless healthcare data integration.
Build and manage scalable pipelines for seamless healthcare data integration.
Ensure secure, compliant delivery of healthcare data via pipelines and APIs.
Manage and optimize cloud-based data pipelines with quality checks and issue resolution.
Maintain system stability, resolve high-severity issues, and optimize platform performance.
Define product strategy, manage roadmaps, and deliver market-ready, compliant features.
Want to discuss a potential project, we’re eager to hear from you.
In 2021, Abacus Insights partnered with TechKraft Inc. to accelerate its healthcare data operations strategy. Starting with a core team of 10 data engineers, the partnership rapidly expanded to over 85 specialists across Data Engineering, Tech-Ops, QA, Business Analysis, and Project Management — operating within a HIPAA and ISO 27001-compliant Offshore Development Center (ODC) in Nepal.
The collaboration strengthened Abacus’ platform capabilities, ensured regulatory alignment, and improved operational agility. TechKraft continues to support Abacus in delivering secure, high-quality data services at scale — driving business resilience and accelerating time to value.

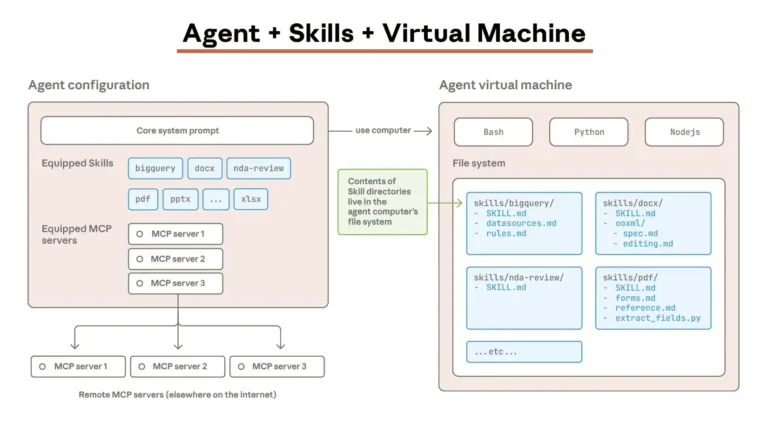
For the past two years, AI development has followed a deceptively simple playbook: stuff everything into the prompt. The logic seemed sound, if Claude can
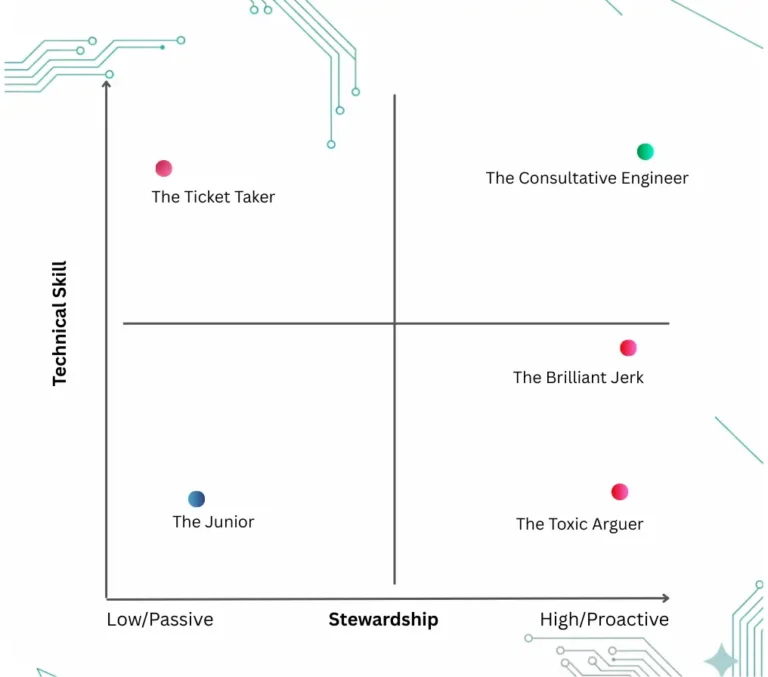
TL;DR Answer: Test Whether Candidates Will Refuse Impossible Requirements The core hiring insight: Engineers who pass coding tests but silently build impossible requirements are more
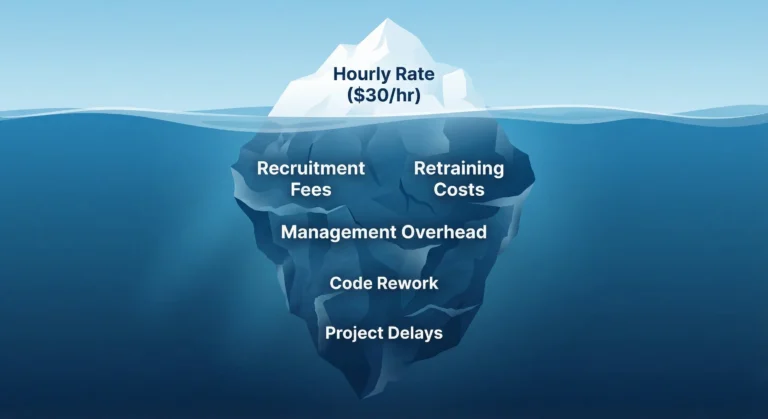
For the past two decades, the offshore narrative has been dominated by a singular variable: cost arbitrage. However, as the digital economy enters a phase
Let us know your needs and discover how we can personalize solutions that best fit your ambition.