In today’s rapidly evolving healthcare landscape, interoperability has become a cornerstone for improving patient care, enhancing clinical decision-making, and streamlining operations. But what exactly is interoperability in healthcare, and why is it so critical?
What is healthcare interoperability
Interoperability in healthcare describes the capacity for disparate health data systems to share data, regardless of geographic location, and allow that data to be used by providers, researchers, and public health managers to improve patient experiences and community health.
Interoperable health systems have their own set of standards and guidelines, with the goal of creating a network of shared health data so that providers can access complete, accurate patient data no matter where the patient has previously received care.
With such a system in place, clinicians can make better decisions and provide better care, patients can take ownership of their data and care options, community leaders can act on early warning signs of public health issues, and finance teams can help ensure prompt and accurate billing and claims reimbursement.
Why Is Healthcare Interoperability Important?
Interoperability enhances healthcare delivery in multiple ways:
- Improved Care Coordination: Providers across hospitals, clinics, and specialists can access up-to-date patient information, reduce treatment gaps, and improve outcomes.
- Reduced Costs: By avoiding redundant tests and procedures, interoperability cuts unnecessary spending and resource use.
- Enhanced Clinical Decision-Making: Access to comprehensive patient histories, including past treatments and medications, leads to more accurate diagnoses and fewer medical errors.
- Streamlined Operations: Automation of data sharing reduces manual data entry and administrative burden, allowing clinicians to focus more on patient care.
- Better Patient Experience: Patients benefit from faster, more accurate care and easier access to their health records, empowering them to participate actively in their care.
Why Achieving Interoperability Remains a Challenge
Despite its clear benefits, healthcare interoperability faces persistent barriers. Below is a detailed breakdown of the core challenges:
1. Fragmented Technology Ecosystems
Proprietary System Lock-in: Many organizations use legacy EHRs, payer platforms, and clinical systems that store data in isolated, vendor-specific formats. This creates “data silos” where critical patient information cannot flow freely between systems.
Limited Standardization Support: Older systems often lack native support for modern data standards (e.g., FHIR, HL7), forcing costly custom integrations that are brittle and difficult to maintain.
2. Semantic and Structural Misalignment
Inconsistent Data Definitions: Even when APIs exist, differences in how data is categorized (e.g., lab codes, medication names) lead to mapping errors, lost context, or failed integrations.
Legacy vs. Modern Workflow Mismatches: Traditional systems rely on batch processing, while modern care demands real-time exchange—creating delays in critical data availability.
3. Security and Compliance Complexities
Evolving Regulatory Requirements: Sharing sensitive health data requires adherence to HIPAA, GDPR, and regional laws, which vary globally. Legacy systems lack built-in mechanisms for audit trails, encryption, or patient consent management.
Cybersecurity Vulnerabilities: Older protocols (e.g., HL7 v2) were not designed for today’s threat landscape, requiring additional security layers that increase costs and complexity6.
4. Operational and Financial Barriers
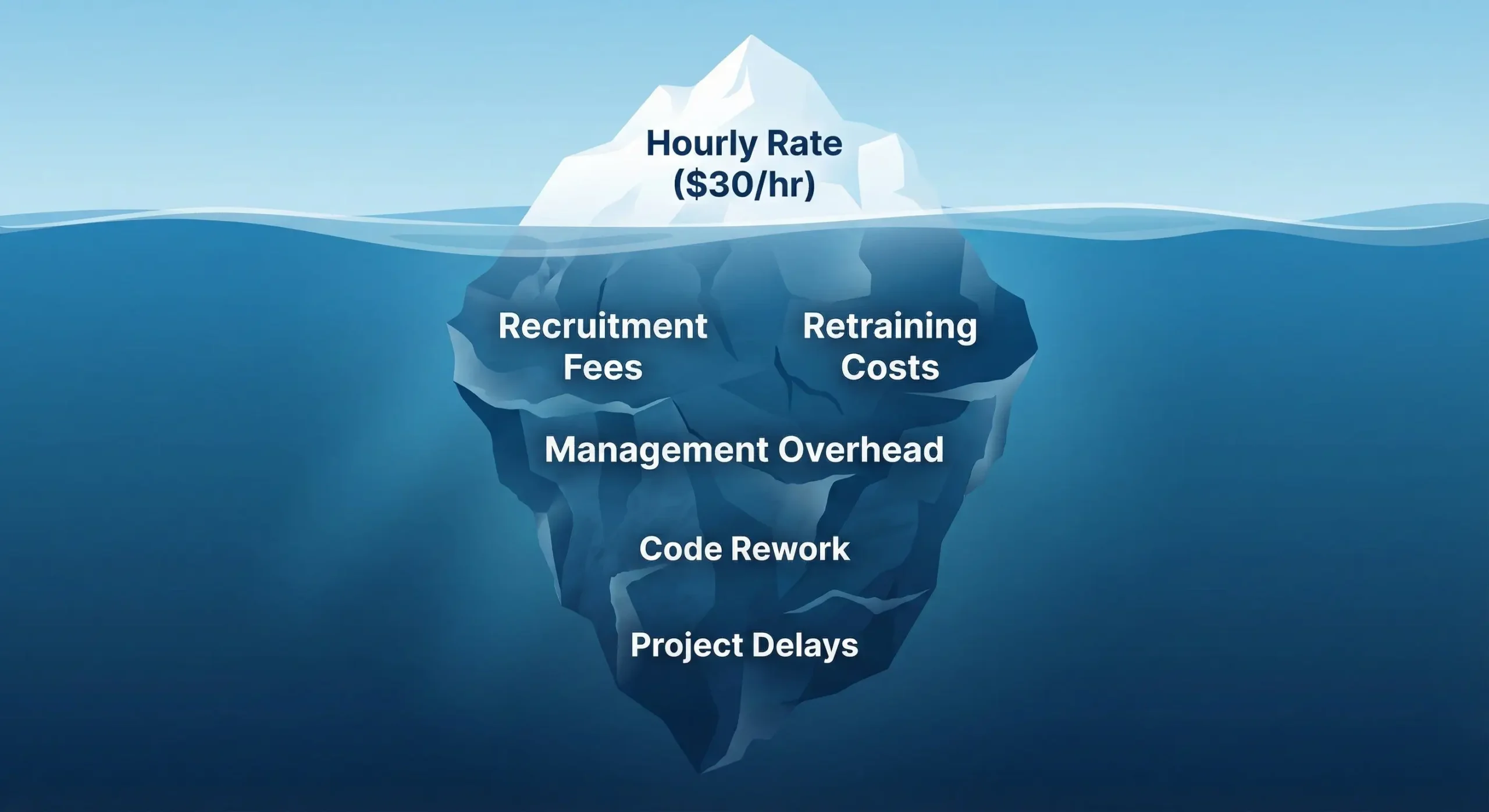
High Implementation Costs: Retrofitting legacy systems for interoperability demands specialized developers that are scarce and expensive, custom interfaces, and ongoing maintenance.
Workflow Disruption Fears: Providers resist changes that may slow down clinical operations or require retraining, especially when ROI is not immediately visible.
5. Organizational and Governance Hurdles
Data Ownership Disputes: Competing priorities between hospitals, vendors, and payers lead to restrictive data-sharing policies and reluctance to collaborate.
Lack of Standardization Enforcement: Without universal adoption of modern standards (e.g., FHIR), even willing organizations struggle to achieve seamless exchange.
6. Technical Debt and Legacy Infrastructure
Outdated Architectures: Many systems predate cloud-native design, APIs, and scalable microservices, making them incompatible with modern interoperability demands.
Resource Constraints: Maintaining legacy interfaces diverts IT budgets from innovation to “keeping the lights on,” slowing digital transformation.
What True Interoperability Enables
When fully implemented, interoperability transforms the way healthcare systems operate. It makes care coordination more efficient, eliminates administrative friction, and empowers real-time data sharing that supports both clinical and operational decisions.
Interoperability significantly improves patient safety by providing clinicians with access to a patient’s longitudinal medical history, including allergies and prior diagnoses. This access helps mitigate adverse drug interactions and clinical errors. For example, participation in Health Information Exchanges (HIEs) has been shown to identify high-risk medication use that might otherwise go unnoticed.
Evidence of Impact: Global Perspectives
A global study involving healthcare providers, administrators, digital health vendors, and patients across 24 countries found that over 90% of respondents recognized interoperability’s positive impact on patient outcomes. Benefits included improved care coordination, reduced medical errors, and enhanced data accuracy. Real-world improvements cited were reduced hospital readmissions and better chronic disease management.
TechKraft’s Role in Solving Interoperability Challenges
TechKraft has been a trusted partner for healthcare platforms seeking to modernize their data infrastructure. Our work spans API development, cloud engineering, and AI-powered automation that is always with a strong focus on security, compliance, and patient data integrity.
We specialize in building FHIR-native interfaces that align with CMS mandates, supporting integrations across EHRs, payer systems, and digital health platforms. Our teams have deep experience designing secure data pipelines for healthcare analytics and claims automation, all built on HIPAA and ISO 27001:2022-certified frameworks.
TechKraft works closely with each client to architect tailored systems that scale securely and adapt to evolving regulatory requirements. Whether the goal is to streamline prior authorization, improve payer-provider data exchange, or support patient access APIs, our solutions are built to deliver lasting value.
Final Thoughts & Next Steps
Interoperability is no longer just an IT initiative but a strategic priority for healthcare leaders who want to drive efficiency, reduce risk, and improve patient outcomes.
As the healthcare ecosystem becomes more connected, the organizations that succeed will be those that treat data not as a siloed asset, but as a shared resource.
At TechKraft, we bring together technical expertise, domain experience, and a proven track record of healthcare engineering success. If you’re exploring ways to modernize your data infrastructure, meet CMS mandates, or automate prior authorization workflows, we’re ready to help. Schedule a meeting today.